Endometriosis is a chronic uterine disorder that causes tissue resembling the uterine lining (endometrium) to grow in areas outside the uterus. This misplaced tissue can attach to the ovaries, fallopian tubes, the outer surface of the uterus, and even other organs in the pelvic cavity like the bladder or intestines. Unlike normal endometrial tissue, this tissue outside the uterus has no way to exit the body, so it builds up, breaks down, and bleeds with each menstrual cycle.
As a result, women with this pelvic inflammatory condition often experience intense pelvic pain, especially during menstruation. Many also report pain during ovulation, sexual intercourse, bowel movements, or urination—depending on where the tissue implants itself. Over time, the repeated inflammation can lead to scar tissue, adhesions, and ovarian cysts (endometriomas), which may distort reproductive anatomy.
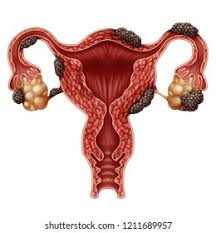
In more advanced cases, endometriosis interferes with fertility by blocking the fallopian tubes, damaging eggs, or disrupting hormonal signals essential for conception. Although the severity of symptoms can vary, even mild cases can severely impact a woman’s quality of life and reproductive health.
If you notice persistent pelvic pain, heavy menstrual bleeding, or difficulty conceiving, you should consult a gynecologist for evaluation and management of this reproductive health condition.
Common Symptoms of Endometriosis
The symptoms of endometriosis can vary in severity and may even be mistaken for other conditions. Some women may experience no symptoms at all. However, the most common signs include:
- Pelvic pain, especially during menstruation
- Pain during intercourse
- Pain with bowel movements or urination
- Excessive menstrual bleeding
- Infertility
- Fatigue, diarrhea, constipation, bloating, or nausea, particularly during menstrual periods
If you’re experiencing any of these symptoms consistently, it is advisable to consult a gynecologist.
What Causes Endometriosis?
The exact cause of endometriosis is still unknown, but several theories exist:
- Retrograde menstruation: Menstrual blood flows backward through the fallopian tubes into the pelvic cavity.
- Embryonic cell transformation: Hormones like estrogen may transform embryonic cells into endometrial-like tissue.
- Surgical scar implantation: After surgeries like a hysterectomy or C-section, endometrial cells may attach to the surgical incision.
- Immune system disorders: A faulty immune system may fail to destroy endometrial tissue growing outside the uterus.
Genetics, hormonal imbalances, and immune system dysfunction are all believed to play a role in the development of endometriosis.
How is Endometriosis Diagnosed?
Diagnosing endometriosis can be challenging due to its similarity to other conditions like irritable bowel syndrome (IBS) or pelvic inflammatory disease (PID). Common diagnostic methods include:
- Pelvic examination
- Ultrasound imaging
- Magnetic Resonance Imaging (MRI)
- Laparoscopy (a minor surgical procedure used to view endometrial tissue directly)
Laparoscopy is considered the most definitive method for diagnosing endometriosis.
Treatment Options
Managing chronic pelvic disorders like endometriosis often requires a multifaceted approach. Treatment is typically personalized based on the severity of symptoms, the patient’s age, and fertility goals. Below are the most effective treatment strategies available today:
1. Medications
For many women, the first line of defense against this reproductive health condition includes medications to relieve pain and regulate hormonal balance.
- Pain Relievers:
Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen are commonly prescribed to reduce menstrual cramps, pelvic pain, and inflammation caused by the condition. - Hormonal Therapy:
Because uterine inflammatory disease is driven by hormonal fluctuations—particularly estrogen—hormonal treatments can help shrink or suppress abnormal tissue growth. Options include:- Oral contraceptives (birth control pills) to regulate or halt menstruation
- Progestins to thin the endometrial tissue
- Gonadotropin-releasing hormone (GnRH) agonists, which lower estrogen levels and induce a temporary menopausal state to reduce symptoms
- In summary, these therapies aim to relieve pain and slow the progression of the disease, though they may not improve fertility directly.
2. Surgery
When medications fail or when symptoms severely affect quality of life, surgical options may be recommended.
- Laparoscopic Excision Surgery:
This minimally invasive procedure involves using a laparoscope to identify and remove endometrial-like tissue growing outside the uterus. It’s considered the gold standard for treating moderate to severe cases while preserving reproductive organs, making it a suitable option for women hoping to conceive. - Hysterectomy:
In extreme cases where the reproductive health disorder is unresponsive to other treatments and fertility is no longer a concern, a total hysterectomy (removal of the uterus, and sometimes the ovaries) may be advised. However, this is typically viewed as a last resort.
3. Lifestyle Changes
In addition to medical or surgical treatments, adopting a healthier lifestyle can play a supportive role in managing this female pelvic condition.
- Regular Exercise:
Engaging in low-impact activities like walking, swimming, or cycling can reduce pelvic pain and lower estrogen levels naturally. - Balanced Diet:
Consuming an anti-inflammatory diet rich in fruits, vegetables, omega-3 fatty acids, and whole grains may help alleviate symptoms. - Stress Management:
Chronic stress can worsen symptoms of endometriosis. Therefore, practicing relaxation techniques such as yoga, meditation, or deep breathing exercises may improve both mental and physical well-being.
4. Fertility Treatment
For women struggling with infertility due to this reproductive tract disorder, specialized fertility treatments are often necessary.
- Assisted Reproductive Technologies (ART):
In cases where natural conception is difficult, procedures such as in vitro fertilization (IVF) or intrauterine insemination (IUI) offer a viable path to pregnancy. Moreover, surgical removal of endometrial growths prior to ART can increase the chances of success.
Ultimately, while endometriosis can complicate the journey to parenthood, modern medical advancements and early intervention provide many women with hopeful outcomes.
Endometriosis and Fertility
A reproductive health disorder like endometriosis directly affects a woman’s fertility by disrupting the normal function of her reproductive organs. This chronic uterine condition triggers inflammation and causes the body to form scar tissue and adhesions. These abnormal tissues often grow around the ovaries, fallopian tubes, and uterus, making it harder for these organs to function properly.
The body struggles with ovulation, fertilization, and embryo implantation when these structures don’t work as they should. In many cases, women experience blocked fallopian tubes or poor egg quality due to the ongoing inflammation and damage. Medical studies show that 30% to 50% of women with this pelvic inflammatory condition face fertility challenges.
However, not every woman with endometriosis becomes infertile. Many conceive naturally or through assisted reproductive technologies (ART) such as IVF, especially when they receive early diagnosis and proper treatment. By taking action early, women can improve their chances of conception and reduce long-term complications linked to this condition.

Nevertheless, not all cases result in infertility. In fact, many women with mild to moderate endometrial disease can still achieve pregnancy.Either naturally or through assisted reproductive technologies (ART) such as intrauterine insemination (IUI) or in vitro fertilization (IVF). Furthermore, with early diagnosis and proper management—including laparoscopic surgery to remove lesions—reproductive outcomes can be significantly improved.
Therefore, if you’re struggling to conceive and suspect underlying symptoms like pelvic pain or irregular menstruation, it’s essential to consult a fertility specialist or gynecologist for timely evaluation and treatment options.
FAQs
Q: Is endometriosis a life-threatening condition?
A: No, but it can severely affect your quality of life and may lead to complications like infertility or chronic pain.
Q: Can endometriosis go away on its own?
A: Rarely. Most women require treatment to manage symptoms effectively.
Q: Is pregnancy a cure for endometriosis?
A: No, pregnancy may temporarily ease symptoms, but it is not a cure.
Conclusion: Don’t Ignore the Signs
Endometriosis, a chronic reproductive disease, affects millions of women and often goes undiagnosed for years due to its complex This condition causes tissue similar to the uterine lining to grow outside the uterus, leading to inflammation, scarring, and severe pain. Because the symptoms often resemble those of other conditions, many women struggle to receive an accurate diagnosis in time.
Recognizing the signs early becomes essential. Women with this chronic pelvic disorder often report persistent pelvic pain, heavy menstrual bleeding, pain during intercourse, and difficulties with conception. When you stay alert to these symptoms, you give yourself a better chance at early diagnosis and effective treatment.
Healthcare professionals can distinguish endometriosis from other conditions like ovarian cysts, pelvic inflammatory disease. Unlike temporary solutions, a clear diagnosis allows doctors to tailor treatments based on your specific symptoms and reproductive goals.
You can manage this uterine health condition by following a comprehensive treatment plan. Doctors may recommend pain relief medications, hormonal therapies, or minimally invasive surgeries to remove abnormal tissue growths. In many cases, women who follow their treatment plan experience significant relief from symptoms and a noticeable improvement in their daily lives.
If you notice ongoing menstrual irregularities, sharp pelvic discomfort, or unexplained fatigue, don’t ignore these signs. Schedule a visit with a gynecologist or a reproductive health specialist immediately. Acting early can help you manage the condition more effectively and prevent further complications, especially if you’re trying to conceive.
In the long term, staying proactive about your uterine and hormonal health allows you to control your symptoms, protect your fertility, and improve your overall well-being.You want to know about Biosurgico then visit Facebook.
